What is the Street Medicine™ Institute?
The Street Medicine Institute (SMI) facilitates and enhances the direct provision of health care to the unsheltered homeless where they live. SMI does this by providing communities and clinicians with expert training, guidance, and support to develop and grow their own Street Medicine programs. SMI has become the global leader in developing the field and practice of Street Medicine and has helped cultivate or improve Street Medicine programs in over 140 cities in 27 countries across 6 continents. SMI is also a membership community that enables professionals and other individuals interested in the Street Medicine movement to come together to provide peer support, share best practices, seek advice and learn about key concepts necessary for a successful Street Medicine program.
Our Mission
Inspiring and equipping communities worldwide to provide Street Medicine services to persons experiencing rough-sleeping homelessness.
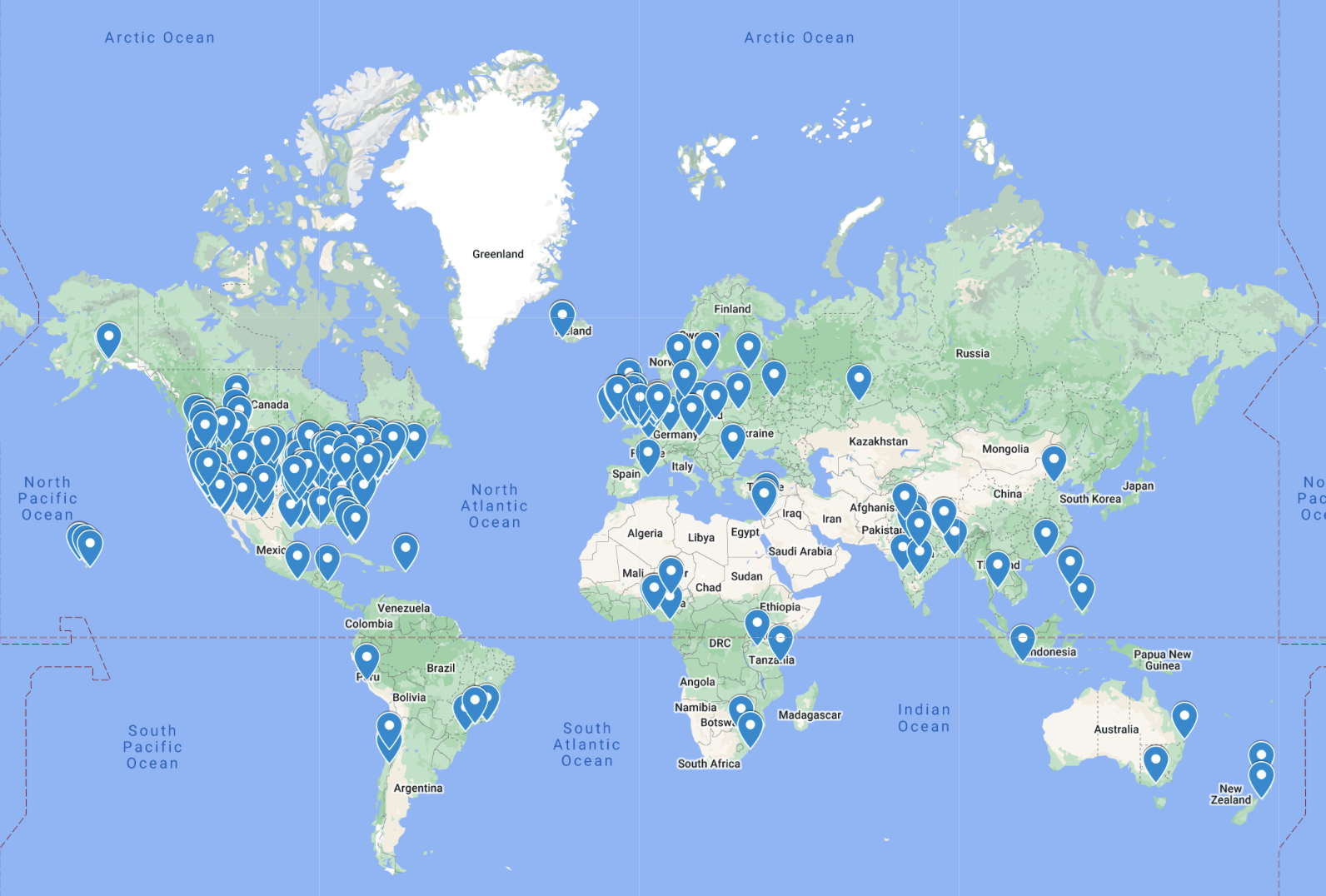 Street Medicine Around the World
Street Medicine Around the World
This map depicts all street medicine efforts known to the Street Medicine Institute, including those where Street Medicine Institute leaders have engaged in collaborative efforts toward the development and improvement of Street Medicine Programs.

Thank You to Our Supporters